Macular Hole
What causes a macular hole?
The central part of the retina is called the macula and the most central part of the macula is called the fovea. The fovea is so thin it is sometimes prone to develop problems. Thin wisps of scar-like tissue can pull the edges apart and create a macular hole.
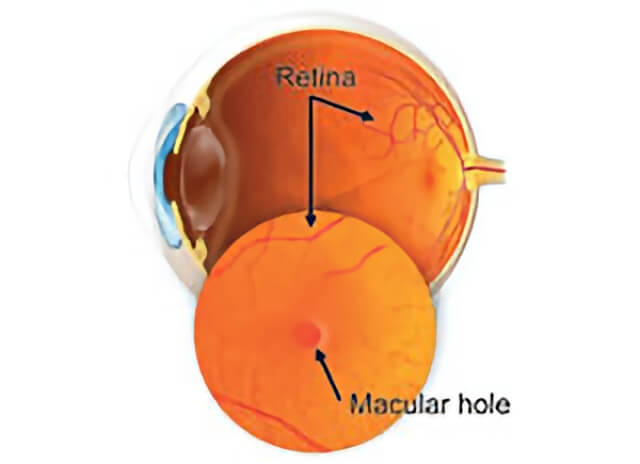
A macular hole forms in the center of the retina in the back of the eye.
Learn more about macular holes at ASRS
Información en español en el sitio web de ASRS
What are the symptoms of a macular hole?
In the early stages, vision becomes blurred and distorted. Over time, a macular hole may progress such that only the “Big E” is visible on the eye chart. Rarely, a macular hole occurs in both eyes.
What testing might be done?
Your doctor will examine your eye and may obtain photographic tests to determine the extent of damage from a macular hole.
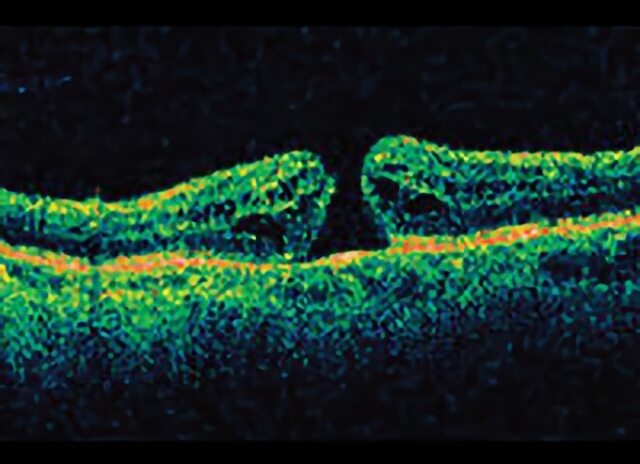
Open macular hole on side view from a special OCT imaging machine.
How is a macular hole treated?
The vitrectomy surgery technique to repair a macular hole was invented in our practice more than 15 years ago. The scar-like tissue is first delicately removed from the surface of the macula. Then, the eye is filled with a special gas bubble that dissolves in about two weeks. You will need to maintain a face down position for about five days to gently compress the tissues back together and allow the hole to close.
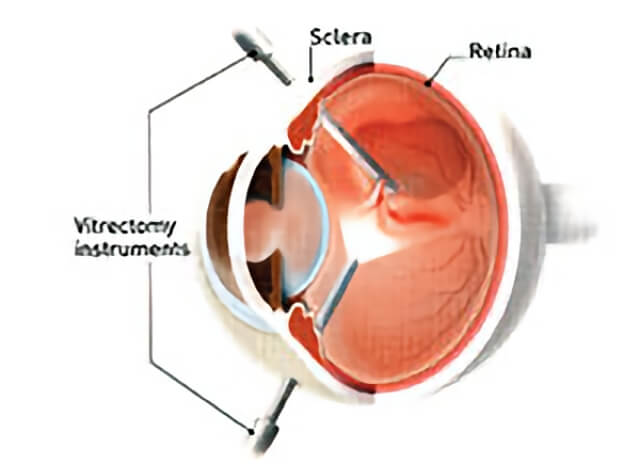
Macular holes are treated with a microsurgical technique called a vitrectomy.
Can the gas bubble put in my eye at the surgery be harmful?
A wristband will alert other medical professionals that you have gas in your eye. A rapid increase in altitude can cause a dangerous rise in eye pressure, so travel in the mountains or by airplane must be avoided. Your surgeon will give you special instructions that will best suit your particular needs.
What can I expect for my vision?
Successful closure of the macular hole approaches 100%, but vision often depends on how long the hole was present before surgery and may not return entirely to normal. We do expect vision to be vastly superior to what it would be if the problem is ignored. Many patients will eventually need cataract surgery and adjustment of their glasses to obtain their best vision after macular hole surgery.
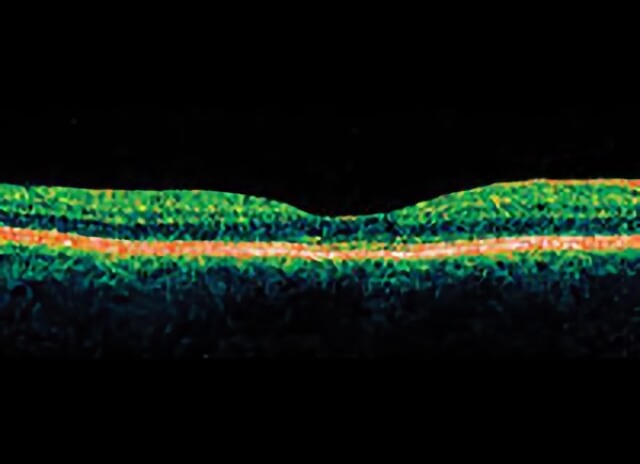
Closed macular hole after successful surgery.
What if I cannot remain in a face-down position after the surgery?
If you cannot remain in a face-down position for the required period after surgery, vision recovery may not be successful. People who are unable to remain in a face-down position for this length of time may not be good candidates for a macular hole surgery. However, there are a number of devices that can make the “face-down” recovery period easier on you. There are also some approaches that can decrease the amount of “face-down” time. Discuss these with your doctor.
Is my other eye at risk?
Patients who have a macular hole in one eye are more likely than the average person to have a macular hole in the other eye. The risk of developing a macular hole in the other eye is around 10-15%. The risk is lower if a posterior vitreous detachment (PVD) is already present in the eye. Ask your retina specialist about your individual risk.


